Darkness Visible, 30 Years Later
Taking Mental Care of Yourself
New Developments in Mental Health Medication
World Autism Awareness
Darkness Visible, 30 Years Later
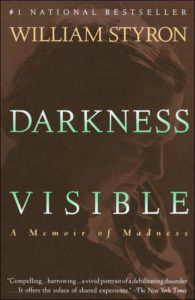
(Vintage Books; 1992)
In 1985, Pulitzer Prize-winning author William Styron nearly ended his own life.
Styron had a distinguished career. The author of Sophie’s Choice and The Confessions of Nat Turner, Styron was a respected literary figure and had been for over a decade when he traveled to Paris to accept a prestigious literary award. From October through December 1985, Styron descended downward in his own depression, and actively considered a suicide attempt. He survived, and the work of nonfiction that came out of it was Darkness Visible.
The title, aptly, is from Milton’s epic poem Paradise Lost: “No light; bur rather darkness visible, served only to discover sights of woe…” Styron chose the phrase, describing Milton’s Hell, as a downward fall into a dark abyss. He was in a beautiful city, Paris, accepting an award for his work. He was in the light, at his top. And yet his mental affliction gripped him, sent him downward. He spiraled toward what he was sure was his end. Depression had found him, and it wouldn’t let go.
Styron first described his story at a symposium for affective disorders at the Johns Hopkins School of Medicine in May 1989. It was published in Vanity Fair in December 1989, and Random House published it as a full-length memoir entitled Darkness Visible in 1990. At only 100 pages, it still resonated with readers. Styron describes painful episodes of sadness, fatigue, lack of concentration, and a total loss of pleasure in his life; he’s gripped by suicidal ideation. He has all the hallmarks of a major depressive episode, and tries several unsuccessful methods to treat it. In between, he discusses famous sufferers of depression, such as Abraham Lincoln and Primo Levi, the latter an award-winning Holocaust survivor and author who had taken his own life in 1987.
Styron describes working with a doctor named Dr. Gold, trying Group Therapy, and various medications. His wife supports him throughout his ordeal. He fantasizes about suicide as his treatments continue to fail, until he is admitted to a hospital in December and begins to make his recovery. As Styron gradually comes out of his depressive episode, he reflects on the illness and what it means, not only to himself, but to others. He considers the multitude of famous creatives who have suffered from the disorder, and wonders if there is a correlation between creativity and depression. His conclusion was that there is. He similarly discusses the unfair stigma attached to mental illness, which unfortunately persists to this day.
“Calling ‘Chin up!’ from the safety of the shore to a drowning person is tantamount to insult,” Styron wrote, referring to those who offered platitudes but no real help. He captures moments that, for many depression sufferers, are almost universal: the cycles of anxiety and sadness; complete fatigue, and yet an inability to sleep; uncontrollable misery, lack of pleasure in most things. What Styron did thirty years ago is something we still attempt to do now: bring attention to a prevalent, destructive condition. Andrew Solomon famously referred to it as The Noonday Demon in his book of the same title, and it fits as an analogy: a creeping presence that can possess us, destroy lives. The stigma attached to it comes from a lack of understanding and empathy, not a lack of evidence.
We’ve come further in thirty years toward understanding and empathy. We now treat depression as not only a mental affliction, but a physical one as well. It can affect anyone. There isn’t a cure or immunity to it. Styron’s journey is something many of us will face—more than 16.1 million American adults aged 18 and older in a given year suffer from major depressive disorder. At Alivation Health, we hear daily about similar struggles ordinary people face. We’ve treated many like William Styron.
What still resonates all this time, thirty years later, are the precipitous highs and lows Styron encountered. He descended as deeply as he could go—but he returned. Unlike in Milton, the light came back to him, and Styron survived to write about his experiences for the benefit of others. Depression often makes you feel alone in the dark, grappling for anything, afraid. But by emphasizing his experience, and highlighting the journey, Styron helped bring light to others from their chasms. The best thing we can do for mental health is to communicate and educate, and by doing this we empathize and learn. We can kill the stigma, encourage others to speak out and seek the help they need. Knowledge, the world over, brings an end to visible darkness.
Taking Mental Care of Yourself

It’s become a cliché to refer to “mental health days”, those days when you don’t work, relax, work on yourself in whatever way you want. A day of Netflix and sleeping, perhaps, or doing activities you don’t always have time for. Many of us have used the phrase, but not all of us have really digested what it means and the actual scientific and psychological good it can do for overall well-being. There’s great value to taking your mental health as seriously as you’d take any illness.
Psychological well-being and a healthy mind don’t always have to be heavy topics. In fact, it’s often best if they aren’t. For many of us, the best treatment for a stressed mind is to pursue a hobby or an activity we’re fond of. Maybe a day off is a good time to catch up on reading, or work out, or just binge a TV show we’re further behind on than we’d like to admit. We often forget about the value of artistic pursuits in a world of demands and tight schedules. Work and play are meant to go together in doses, but we often neglect one in favor of the other. Such are the demands of the modern world that we don’t have time for everything, and must prioritize our days around what we need.
Insert the mental health day.
It isn’t weak to work on yourself, your emotional and mental health, or your psychological well-being any more than it’s weak to work on getting over the flu. Overworking yourself can lead to exhaustion. It doesn’t always entail taking a day off from work—often it just means setting aside time for your own pursuits. The weekend can be a great time for that, especially in spring and summer when we’re able to enjoy outdoor activities and the sun. Nothing rejuvenates faster than stopping to smell the proverbial flowers.
Some of the other best things include getting a good night’s rest, which many Americans lack. Insufficient sleep is associated with numerous chronic maladies, ranging from diabetes and cardiovascular disease to high blood pressure and mood disorders. A day of sleep isn’t a bad idea in this case. Many of us enjoy the peace and quiet that come with full rest, and if it has physical benefits as well, then the more the merrier.
Other beneficial suggestions include socializing, especially with other friends who could use a meaningful connection, or have their own mental health challenges and would appreciate the reach-out. In a constantly-wired world, sometimes unplugging and having old-school communication can switch up your paradigm. We like pleasant changes that accent our days, and having positive outlets like friends is one of the best things we can use.
Other common suggestions include eating healthy and exercising. These, of course, can help mental health tremendously. Exercise is well-known for its immense psychological benefits. But sometimes it’s also rewarding to indulge in something purely for the pleasure of it, such as ice cream or chocolate. Don’t worry about that last one—chocolate, specifically extra dark chocolate, seems to also be good for your brain, in the right doses. Moderation is the key to everything, including the things we love.
The real point of all this—and mental health care in general—is to just set aside time to do the things you love. If it makes you happy, try to fit it into your day, or find a day when you can pursue it the way you want. It’s an excellent way to depressurize yourself, focus on personal well-being, and not only positively influence your own health, but the health of those around you. A good mood can be contagious, and who doesn’t want their mental health improved to the Next Level?
Especially, of course, if chocolate can be involved.
New Developments in Mental Health Medication

It’s an exciting time for mental health treatment.
You may have heard, but in the past six weeks, the FDA has approved new medication for treating depression and postpartum depression. In the latter case, this marks the first time ever a drug has been approved and marketed specifically for that condition.
The drug is an intravenous infusion called brexanolone, which will be sold as Zulresso. What makes the medication so notable is the speed in which it works—whereas conventional antidepressants can take days or weeks to have effects, brexanolone was shown in clinical trials to take effect within hours. That’s an incredible achievement, and a wonderful boon to new mothers, one in nine of whom suffer from postpartum depression. The medication will become available in June.
There are drawbacks, however. Zulresso was approved with a REMS (Risk Evaluation and Mitigation Strategy), meaning it’s only available to patients through restricted distribution programs at certified health care facilities. At these facilities, the health care providers can carefully monitor the patient for as long as necessary. Brexanolone is administered in a 60-hour IV drip, comes with side effects such as headache or dizziness, and, according to Sage Therapeutics, will likely cost around $20,000 to $35,000 per treatment.
What’s truly unique about brexanolone is that there are no other FDA approved antidepressants for postpartum depression. This is a first of its kind. There will undoubtedly be further developments and exciting new treatments in the future, but progress starts with a single step. Without treatment, postpartum depression can last for months or, sometimes, years. It can negatively impact the quality of life for new mothers and their infants. Treatments that alleviate that, and so quickly, are the goal of all mental health medication research.
The other medication that was approved is called esketamine, a nasal spray used in conjunction with an oral antidepressant. It’s the first new treatment for depression to be approved by the FDA in over thirty years. Alivation Health has been offering standard ketamine treatment for many years. Since the approval of esketamine, we’ve been asked about it many times. We are able to provide esketamine as a treatment option, however, since it is not covered by most insurance plans today, it is much costlier than the ketamine we continue to provide. Alivation is focused on working with insurance companies so that hopefully in the future, esketamine will be more widely covered.
The two medicines, ketamine and esketamine, have not been compared to one another in large-scale clinical trials, but their effects are known to be quite similar. Neither have long-term addiction or habit-forming effects. They both have excellent potential uses for treatment-resistant depression, making them very valuable to those suffering that condition.
The future seems a little brighter for those suffering from depression. New treatments are being tested and studied every day, and occasionally, as has happened in the last few weeks, they’re also approved. Increasing varieties of treatment options and competition in this area may eventually allow prices to go down, and the patient will be the one benefitting the most. And that’s what treatment is all about.
World Autism Awareness

Yesterday was the twelfth annual World Autism Awareness Day, and all of April is World Autism Month.
What is autism?
From Autism Speaks: “Autism, or autism spectrum disorder (ASD), refers to a broad range of conditions characterized by challenges with social skills, repetitive behaviors, speech and nonverbal communication. Autism affects an estimated 1 in 59 children in the United States today.”Autism is a spectrum disorder, meaning there are many subtypes, often influenced by environmental and/or genetic factors. It ranges in severity from highly skilled to severely challenged. Indicators of autism often appear by age two or three. The common ones, from the Global Autism Project, are:
- Delay and/or difficulty in learning language or lack of functional communication.
- Children on the autism spectrum disorder typically have some degree of impairment in communication. They may not respond to their name, initiate interaction with others, or demonstrate age-appropriate language development.
- Individuals with autism may often engage in repetitive body movements.
- Hand-flapping, tapping, spinning/rocking their body, or looking at things out of the corner of their eye.
- Marked impairments in interpreting and reciprocating non-verbal gestures.
- May demonstrate difficulties in identifying and interpreting various facial expressions and body-language such as foot tapping, stares, discomfort, raised eyebrows, etc.
- May focus on restricted interests.
- This can include preoccupation with certain topics or having things a certain way—like wanting to learn everything about vacuum cleaners or lining things up in a certain order.
- Lack of interest or deficits in developing and maintaining peer appropriate relationships and delayed development of social skills.
- As stated, while some individuals on the spectrum prefer solitude, many desire to make friends, interact socially but may lack the functional ability to do so (aka hidden curriculum).
- Many people on the spectrum may appear shy, standoffish, or unaware of those around them.
There has been some confusion about autism. While there are many questions about the genetic and environmental causes of autism, and much research in this area, we do know what likely doesn’t cause autism: the MMR vaccine. The only study ever to link the MMR (Measles, Mumps, Rubella) vaccine to autism was a small, fraudulent study conducted by Andrew Wakefield that was officially and fully retracted by The Lancet, the journal that initially printed it. Medical researchers have stressed repeatedly that connections between the MMR vaccine, thimerosal, and autism are a myth. The American Academy of Pediatrics, so frustrated by this false, persistent link, has even compiled a comprehensive list of the many, many studies done testing the correlation—not one of which found any connection at all.
Here’s what we do know about the causes of autism: it tends to run in families; there is an increased risk for it with advanced parent age (either parent); pregnancy or birth complications and pregnancies spaced less than one year apart may also increase the risk. There are no bulletproof ways to prevent autism, but there are many treatment options available.
Here’s what we also know about autism: it deserves support and compassion. It deserves your understanding and your knowledge. It needs your help to raise awareness about its complications, not only for the individual with autism, but also for the family and the caregivers. The disease can often be emotionally and physically taxing. Those with autism can struggle to integrate with other children or adults, or utilize social cues and skills. For many of us, we often take for granted what for others is an enormous challenge. This year for World Autism Month, spread social media hashtags and articles raising awareness; read and learn about the realities of autism and what you can do to help. Understand the challenges those with it and those caring for others with autism face.
The best thing we can do is communicate, educate. The best thing we can do is care.
