Alzheimer’s Disease
Understanding Clinical Depression
Diet and Mental Health
Mental Health in Popular Culture
Alivation’s 2018: A Pictorial Review
Alzheimer’s Disease
Few diseases inspire the kind of mystery and fear that Alzheimer’s does.
Alzheimer’s is ranked as the sixth leading cause of death in the United States, although new estimates suggest the disease may rank just behind heart disease and cancer as a cause of death for older people, according to the Alzheimer’s Association. Alzheimer’s isn’t a normal part of the aging process. It’s the most common cause of dementia among older adults, and approximately 200,000 Americans under the age of 65 have early-onset forms of the disease. Alzheimer’s worsens over time, progressively worsening over the years. Eventually, individuals forget family members, lose the inability to carry on conversations, and respond to their environment at all.
This is what inspires the most dread.
Few things make up the individual like our memories. Our social connections, our familial relationships, and our memories of places and interactions form the core of our experiences. As we age, we naturally behind to forget some of those things. With Alzheimer’s, those experiences aren’t simply discarded or forgotten—they’re stolen. A grandparent, a parent, a friend losing their memory of you, who they are, and where they are is particularly tragic to us in this light. We lose our core selves.
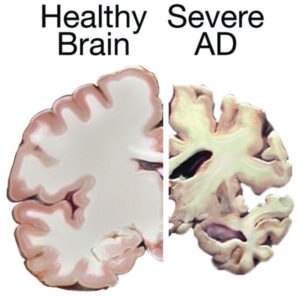
Alzheimer’s is named after Dr. Alois Alzheimer, who, in 1906, noticed changes in the brain tissue of a woman who had died of an unknown illness—an illness that “included memory loss, language problems, and unusual behavior”. Upon studying her brain postmortem, Dr. Alzheimer found abnormal clumps (amyloid plaques), and tangled bundles of fibers, called tau tangles. These are still considered among the main features of Alzheimer’s, along with the loss of connections between neurons in the brain.
Every year, scientists get closer to understanding the illness a little bit better. Damage to the brain is now thought to occur “a decade or more” before cognitive problems begin to appear. Abnormal deposits of proteins form the amyloid plaques and tau tangles throughout the brain, and neurons lose connections with other neurons, and die. This is what causes the progressive memory loss, dementia, and eventually death. Genetically, a gene called APOE is involved in late-onset Alzheimer’s. Carrying a form of this gene does not definitively prove a person will develop Alzheimer’s, and some people even lacking the gene entirely may still develop the disease. Advances in brain imagining are moving us closer to seeing and understanding the illness better than ever, helping track the very earliest steps in the disease process.
As for lifestyle factors, there is a great deal of interest in the link between vascular conditions such as heart disease, stroke, and high blood pressure, many of which bear resemblances to Alzheimer’s. Researchers are currently studying how reducing these risk factors may reduce the risk of Alzheimer’s. In the meantime, a nutritious diet, physical activity, social engagement, and mentally stimulating pastimes are all associated with better health and physical, and mental, longevity, according to NIA.
From the Alzheimer’s Association, Alzheimer’s Disease is diagnosed in some of the following ways:
- Asking the person and a family member or friend questions about overall health, past medical problems, ability to carry out daily activities, and changes in behavior and personality.
- Conducting tests for memory, problem solving, attention, counting, and language.
- Carrying out standard medical tests, such as blood and urine tests, to identify other possible causes.
- Performing brain scans, such as computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET), to rule out other possible causes for symptoms.
If you suspect you or a loved one might have Alzheimer’s, any form from early to late-onset, come in to Alivation as soon as you can. Early detection is essential. With a range of doctors, PAs, and psychologists on staff, we’re able to provide clarity for your ailment, and how best to treat it. We’ll always be with you in your journey to the Next Level.
Understanding Clinical Depression
There are many illnesses in the world with visible symptoms. You get chickenpox, and everyone can see it plainly. The common cold or the flu is visible, too: coughing, sneezing, runny noses, the works that we’ve all had. But what about disorders that aren’t visible? If there are no outward symptoms, how can we know something is wrong?
This is the common challenge of major depressive disorder (MDD).
If you have MDD, you know it. You can’t shake a feeling; you can’t rise out of your feelings of inadequacy, or worthlessness, or sense that nothing is worth it. Your motivation has plummeted. You feel alone, often anxious. You have no energy but can become irritable quickly. Sometimes you can’t even leave the house, and maintaining relationships even with close family members feels like an insurmountable task. It’s like living with cement blocks on your feet, and you’re dragged down every time you try and move away from it.
These are the symptoms depression sufferers know all too well. It isn’t a mystery what’s going on, and your symptoms are as prevalent as any cold to you. It can be completely debilitating. Given the link between suicide and MDD, it can also be fatal. So what’s going on?
Depression isn’t like the flu or chickenpox. It isn’t caused by a virus, and it isn’t found in unclean drinking water. It begins where it lurks: in the brain. The exact causes of depression are not clearly understood. There may well be a variance in the causes from person to person. The current best theory involves monoamine neurotransmitter activity, specifically levels of serotonin. Neuroimaging can show us depression activity in the brain. It isn’t just “in your head”—it’s real, scientifically verified.
There’s nothing worse than being told nothing is wrong with you when, clearly, something is off. For years, depression, and postpartum depression in new mothers, was brushed off, handwaved as something that was in the sufferer’s head in the worst way, i.e. fictional. “You’re fine!” “Just feel better!” Even today, sufferers of MDD still encounter these responses to their challenges. Those without depression, though often well-meaning, can’t understand what it’s like. It simply isn’t part of their daily life.
In the past, it was hard to understand how mood was not in the patient’s control. We’re used to the idea that we can improve ourselves, and that good things make us feel good, and bad things bad. So why didn’t good things help? Why did sufferers feel bad with no outward cause? In many cases, their lives were average, with no remarkable amount of trauma or hardship. How could they feel this way? Were they faking it? Was it for attention, or did they lack the will to improve themselves? We know a lot more now. The medical community began to listen more, and the emergence of new technologies, such as neuroimaging, along with wide swaths of case studies convinced them that what they were seeing was genuine.
Depression isn’t like the flu; you won’t catch it on the subway. It doesn’t obey communicable disease rules. It’s likely genetic, and often found in families. It ranges in severity from mild to debilitating, and the symptoms sometimes lack consistency: many depression sufferers will overeat, while others will not eat enough; many have disrupted sleeping patterns, with some sleeping too much, and others not enough. Episodes can “range in duration from hours to years”. One famous sufferer of depression was Abraham Lincoln. In his day, the disorder was called “melancholy”, and he was characterized by “fits of gloom” and an unknown sickness.
Treating depression isn’t a one-size-fits-all approach. Some people naturally recover on their own. Physical exercise has been known to benefit depression sufferers. The most common treatments for depression are a class of medication called Selective Serotonin Reuptake Inhibitors (SSRI). There are many common, effective brand names for them. Therapy and counseling are also effective for many. For those who’ve tried medications and therapy but have a stronger case of depression, Transcranial Magnetic Stimulation (TMS) is offered at Alivation. It uses targeted magnetic waves on the areas of the brain causing depression. It is enormously effective, and its use is only continuing to expand throughout the country. One new proposed treatment for postpartum depression is called Sage 217, which works on the brain’s gaba system, something no other current treatment does. More research is needed on this interesting medication.
If you’re having any of the following Mayo Clinic-listed symptoms, call us:
- Loss of interest in activities
- Anxiety
- Feelings of worthlessness, sadness, or guilt
- Aches and pains
- Changes in sleeping patterns
- Low energy
- Thoughts of suicide
We’re here to help in any way we can. We offer a variety of treatments, including medications, therapy services, and TMS. For those looking at other options, Alivation Research has conducted countless, in-depth studies on depression and its effects, and likely will have more studies in the future you could participate in. If you have depression, know that you’re not imagining it, and it is a real disorder. But take heart: because it’s real, we’re able to locate and treat it.
You’re not alone.
Diet and Mental Health

The question has been asked: diet and nutrition impact our physical well-being, so do they affect our mental well-being, too?
The answer seems to be yes.
It’s called nutritional psychiatry, and it’s growing every day. The concept is simple: much like a car requires a certain type of fuel to run its best, so does a brain, also an engine, require the right fuel to run its best. We’ve known the body and the mind are integrated for many years, and what one does impacts the other. To lose weight or prevent heart disease, you eat healthy and exercise. That’s also why we set up Alivation the way we did: pharmacy works with primary care, which works with research; when everything runs together, it runs smoother. It makes sense that the same is true of the brain.
What kind of diet exactly are we talking about?
It depends on the research you look at, but a diet that comes up often in the literature is the Mediterranean diet. With its emphasis on vegetables, especially leafy greens, and fruits, fish, legumes, nuts and other heart-healthy fats, the diet is tailor-made for physical well-being. Some studies have shown issues with weight and obesity can lead to negative mental well-being. A healthy diet that sheds excess pounds, the NCBI says, may contribute to a better sense of self, and a healthier outlook on life. Some studies show a direct link between the Mediterranean diet and a decrease in depression, and plant-rich diets to alleviate symptoms of major depressive disorder (MDD). We’re still waiting on longer-term studies to show the benefits of dietary intervention in depression, but early results seem to support the idea that it can indeed have a positive impact from even small changes.
From another angle, it’s been theorized that nutritional deficiencies can contribute to negative mental well-being. Shortages in things like omega-3s, zinc, iron, vitamin D and folate have been linked to depression and anxiety. Many sufferers seem to have diets that lack adequate amounts of these things, as well as essential amino acids. Gut health, especially the probiotic environment, which aids in nutrient absorption, has been linked to the crucial neurotransmitter serotonin (Harvard Health).
Exercise has long been well known as a natural way to fight depression and anxiety as well. According to Psychology Today, strenuous activity releases endorphins, which increase positive activity and feel-good hormones in the brain. With a diet and exercise regime that results in weight loss, the mental health benefits are boosted by the positive changes to body image. Help Guide says some people may also benefit from calming exercises, such as yoga, that practice the mind-body balance and decrease anxiety by focusing on something else.
A plant-rich diet, low in processed foods, sugar and red meat, and higher in fish, nuts and fruits, seems to be beneficial for not only physical well-being but also mental health. The lifestyle changes work best after two to three weeks, when the body naturally begins to reprogram from a “pro-inflammatory” diet. Coupled with physical exercise or increased daily movements, and the changes are magnified.
For those who made a New Year’s resolution of losing weight or living healthier, the science backs up the mental health benefits of doing so, giving you another reason to follow through. Now is the time to make the positive changes that will make 2019 a physically, and mentally, healthful year.
Here are some nutritional and lifestyle tips to get started, courtesy of the Mayo Clinic:
- Eating primarily plant-based foods, such as fruits and vegetables, whole grains, legumes and nuts
- Replacing butter with healthy fats such as olive oil and canola oil
- Using herbs and spices instead of salt to flavor foods
- Limiting red meat to no more than a few times a month
- Eating fish and poultry at least twice a week
- Enjoying meals with family and friends
- Drinking red wine in moderation (optional)
- Getting plenty of exercise
Mental Health in Popular Culture
We don’t do lobotomies at Alivation.
This doesn’t surprise you, right? It shouldn’t. But in the dramatic world of popular culture and entertainment, a lobotomy is the sort of thing commonly practiced in mental health facilities. Just look at One Flew Over the Cuckoo’s Nest. Happens all the time, right?
Well, no.
The simple truth is, so much of our worldview is influenced by what we see on TV, in movies, in the books we read, or the music we listen to. Astute cultural observers have tried to pin down exactly where truth ends and culture begins, or vice versa. Do we make art, or does art just express what already exists? We’re challenged every day here by people’s perceptions and what they expect. We do our best to educate, but sometimes those preconceptions are just too strong, and patients don’t seek help because of what they expect, or seek help based on dramatic but false notions of mental health treatments.
Let’s start with some common ones.
Raise your hand if you’ve seen any of the following TV shows: The Sopranos, Frasier, Monk, 13 Reasons Why, In Treatment, Mr. Robot, and Unbreakable Kimmy Schmidt. Now what about any of the following films: Good Will Hunting, The Prince of Tides, Analyze This, The Perks of Being a Wallflower, A Beautiful Mind, One Flew Over the Cuckoo’s Nest, Girl, Interrupted, Awakenings, Side Effects, What About Bob, The Departed, As Good As It Gets, Ordinary People, or It’s Kind of a Funny Story. I bet you can name even more than this off the top of your head right now.
There is no shortage of therapy and mental health themes in movies. We’ve all seen the trope: main character lying on a couch in a nice office while a (typically beleaguered) psychologist/therapist sits nearby and listens to their problems for an hour, counting down until they can bill it out and move on to the next one. There are usually ample amounts of Freud-by-way-of-Hollywood psychobabble and screenwriter lingo to fill the moments in between the character affectations. Where does this come from?
The answer is more art than science.
In screenwriting, the main goal is to get as much exposition out of the way as simply as possible about our characters. This paves the way for audience identification and the initiation of the plot. In a three-act structure, the first act is exposition/setup, the second act is the longest, with the protagonist beginning their journey and facing obstacles, and the third act is the resolution and climax. You also want to show growth for the character over their journey. This is why many films and TV shows begin with the character in therapy and end with them in therapy, but having learned something about their expressed problem along the way. One character wants something, and there are obstacles to them getting it. That’s how and why we have stories.
Understanding that, we forgive the movies and TV shows for portraying psychology in a not-so-realistic way. It’s a shorthand for the real thing. Actual therapy is more sessions, and active involvement from the patient. It’s more work from everyone involved, but the benefits are also larger than one character having a “revelation moment” at some point in the 90-minute movie. At Alivation, our therapists are much more involved and, we like to think, helpful than the ones in the movies. They certainly enjoy their jobs more, and they care about the people they see.
Depression and suicide are other common themes, especially in films like Prozac Nation and Girl, Interrupted, and for the same basic dramatic reason: it illuminates a character. We identify with those who are troubled, or challenged, or, sometimes, unbalanced. We like interesting people, and screenwriters know that. We don’t expect the portrayals of the field to end any time soon, and we’re always here to clear up misconceptions.
We at Alivation love those same movies and shows, too. We only get concerned when fabricated cultural views get in the way of real help for people who need it. This is our way of asking that you, please, not get your psychological advice from a movie. If you’re having challenges, please call us and set up an appointment today. We’ll show you the reality of treatment and how help is, in fact, reachable.
Alivation’s 2018: A Pictorial Review
Looking back at our great year.














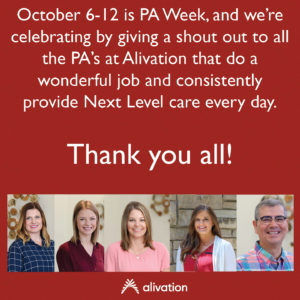









We’re sure 2019 will manage to be even bigger!
